
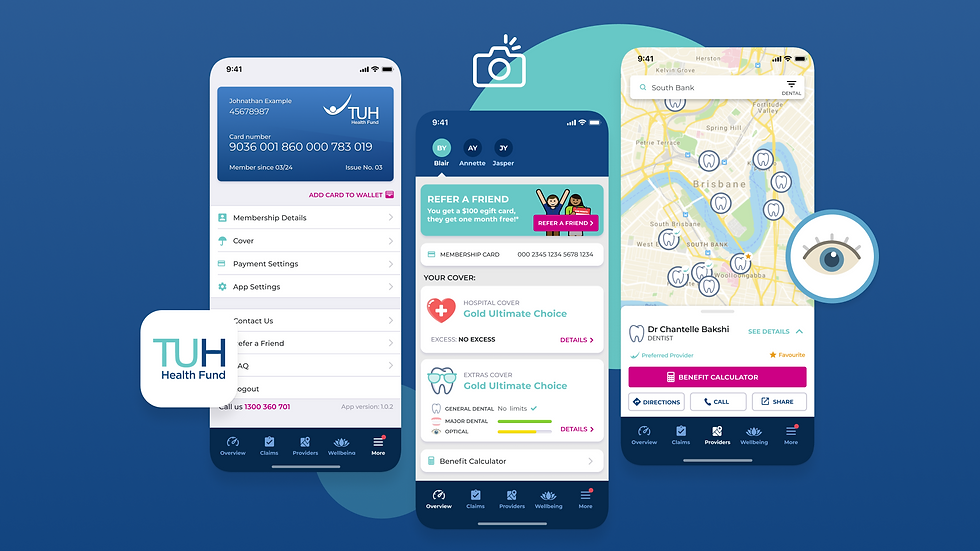
Leading Private Health Fund in Australia
SUCCESS STORY

Since the launch of the app and web portal, TUH Health Fund has witnessed remarkable member engagement. An astonishing 91% of their members have embraced the app, taking control of their health insurance.
Members now have the freedom to access their policy information in real-time, anytime, and from anywhere. This new level of accessibility has not only strengthened the bond between the fund and its members but has also significantly reduced the number of calls and inquiries about policy details.

Since the launch of the app and web portal, TUH Health Fund has witnessed remarkable member engagement. An astonishing 91% of their members have embraced the app, taking control of their health insurance.
Members now have the freedom to access their policy information in real-time, anytime, and from anywhere. This new level of accessibility has not only strengthened the bond between the fund and its members but has also significantly reduced the number of calls and inquiries about policy details.
-
A daily average of 30 address changes processed through the app and portal.
-
An impressive 91% of members using the app.
-
27% of members logging in to the app or web portal each month.
-
900% increase in Express Payments vs Easy Claims
-
Noticeable reductions in simple calls, with most inquiries now centred around complex issues. Call centre team is now more equipped to handle complex and high-priority member issues
-
Considerable time savings in administrative tasks due to single administration system for the app and web portal
-
Reduced claims processing time and errors, leading to improved member satisfaction.
-
Gained full control of critical digital communication channels with members

A daily average of 30 address changes processed through the app and portal.
An impressive 91% of members using the app.
27% of members logging in to the app or web portal each month.
900% increase in Express Payments vs Easy Claims
Noticeable reductions in simple calls, with most inquiries now centred around complex issues. Call centre team is now more equipped to handle complex and high-priority member issues
Considerable time savings in administrative tasks due to single administration system for the app and web portal
Reduced claims processing time and errors, leading to improved member satisfaction.
Gained full control of critical digital communication channels with members
